Pathogenic forms of E. coli can cause diarrhoea, urinary tract infections, pneumonia, and other illnesses. Here is an overview of this bacterial infection.
WHAT IS E. COLI?
Escherichia coli (abbreviated as E. coli) is a type of bacteria that can be found in the intestines of people and animals. Most types of E. coli are harmless and even help to keep your digestive tract healthy. However, others are pathogenic and cause diarrhoea and illness.
Pathogenic E. coli strains are categorised into six pathotypes that are associated with diarrhoea and collectively referred to as diarrheagenic E. coli. There are:
● Shiga toxin-producing E. coli (STEC)
● Enterotoxigenic E. coli (ETEC)
● Enteropathogenic E. coli (EPEC)
● Enteroaggregative E. coli (EAEC)
● Enteroinvasive E. coli (EIEC)
● Diffusely adherent E. coli (DAEC)
STEC may also be referred to as Verocytotoxin-producing E. coli (VTEC) or enterohemorrhagic E. coli (EHEC). This pathotype is the one most commonly heard about in the news in association with food-borne outbreaks. Most cases associated with food poisoning are caused by a strain known as E. coli O157 and people are exposed to it from contaminated water or food . It is often passed on through raw or uncooked meats , but can also be spread through raw vegetables or unpasteurised milk. It can also be transmitted from person-to-person contact.

WHAT ARE THE SYMPTOMS OF E. COLI?
Signs and symptoms of E. coli O157 infection typically begin three to four days after eating or drinking something that contains the bacteria. Illness can, however, start anywhere from one to ten days after exposure.
The most common symptom are:
● Diarrhoea , which may range from mild and watery to severe and bloody.
● Abdominal cramping , pain or tenderness.
● Nausea and vomiting , in some people.
Most healthy people usually start to feel better within a week . People should contact a healthcare provider if diarrhoea lasts for more than 3 days, is accompanied by a fever higher than 39˚C, they have blood in stools, or vomiting prevents them from keeping liquids down.
Around 5-10% of people diagnosed with a STEC infection go on to develop a serious complication called Hemolytic Uremic Syndrome (HUS), which affects the kidneys . This can be life threatening and is more common in young children and the elderly.
HUS typically develops around seven days after symptoms first appear. These symptoms include decreased urine production, dark or tea-coloured urine, and facial pallor.
HOW TO PREVENT E. COLI?
Unlike many other disease-causing bacteria, E. coli can cause an infection even if only small amounts are ingested. This could be from eating an undercooked hamburger or swallowing contaminated water.
Prevention measures include:
● Avoid eating high-risk foods , especially undercooked minced beef, unpasteurised milk or juice, soft cheeses made from unpasteurised milk, or sprouts.
● Use a food thermometer to make sure that minced beef has reached a safe internal temperature of 71° C.
● Wash hands before, during, and after preparing food, after nappy changing infants, and after contact with cows, sheep, or goats, their food or treats, or their living environment.
It’s important to practice good hygiene and hand washing . This will help to prevent transmission from one person to another.
Food safety guidelines should also be followed at all times. The ‘danger zone’ is between 8°C and 60°C so there are a number of best practice steps that can be taken. These include chilling food, ensuring it’s cooked correctly, and avoiding cross-contamination.

WHERE TO FIND MORE INFORMATION?
There are a variety of sources for additional information. The Mayo Clinic provides a good overview of E. coli along with the signs and symptoms, causes and treatment. A similar guide can be found on the WebMD website .
You should also seek advice from governmental food standards. In the UK, this falls under the remit of the Food Standards Agency but recommendations may vary slightly from one county to another. In the US, the Centers for Disease Control and Prevention provides insight as well as a Q&A section and advice for healthcare professionals.
Always follow clinical guidelines and best practice when diagnosing and treating E. coli.

WHAT ARE THE TREATMENT OPTIONS?
The only way healthcare practitioners can know for sure if someone has an E. coli infection is to take a stool sample from the patient and get it analysed.
Fortunately, the infection usually goes away on its own. People are advised to drink plenty of fluids and get rest . If you cannot drink enough fluids to prevent dehydration or if your symptoms are severe (including bloody diarrhoea or severe stomach pain), call your doctor.
For some types of E. coli, antibiotics can shorten the length of time that patients have symptoms and these might be used in moderately severe cases . However, antibiotics shouldn’t be taken if the STEC variety is suspected. That’s because antibiotics can actually increase the production of Shiga toxin and worsen your symptoms.
In most cases, people shouldn’t take over-the-counter medications that fight diarrhoea. It is not advisable to slow down your digestive system because that will delay the body’s shedding of the infection.
When starting to feel better, patients should ideally stick to low fibre foods such as crackers, toast, eggs, and rice. Dairy products and foods that are high in fat or fibre can make your symptoms worse, so these should be reintroduced gradually.

ARE THERE ANY VULNERABLE GROUPS?
As with any food-borne illness, E. coli can affect anyone who is exposed to the bacteria. Most people develop only mild to moderate symptoms and it goes away on its own. Diarrhoea and sickness can cause dehydration , so it’s important to replenish lost fluids.
Some people are more likely to develop problems than others though. Young children and older adults have a greater risk of developing kidney failure brought on by HUS.
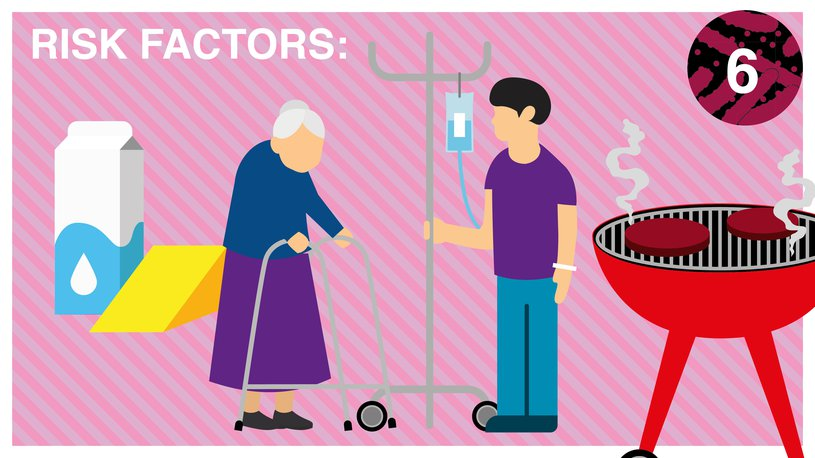
Risk factors include:
● Age. The elderly, young children and infants are at higher risk of experiencing illness caused by E. coli and more serious complications from the infection.
● Weakened immune systems . For example, people with AIDS or being treated with drugs to treat cancer or prevent the rejection of organ transplants.
● Eating certain types of food . Riskier foods include undercooked beef burgers, unpasteurised milk, apple juice or cider; and soft cheeses made from raw milk.
● Time of year . Seasonality plays a part and people are more likely to become infected during the summer months due to under-cooked meat on the BBQ.
● Decreased stomach acid levels . Stomach acid offers some protection against E. coli. Patients that take medications to reduce your levels of stomach acid may have an increased risk of an E. coli infection.
WHAT PRODUCTS ARE EFFECTIVE?
Pal Hygiene has three ranges of products effective against E. coli.
- Hand Sanitising Wipes
- Alcohol Surface Disinfectant Wipes
- Surface Disinfectant Wipes

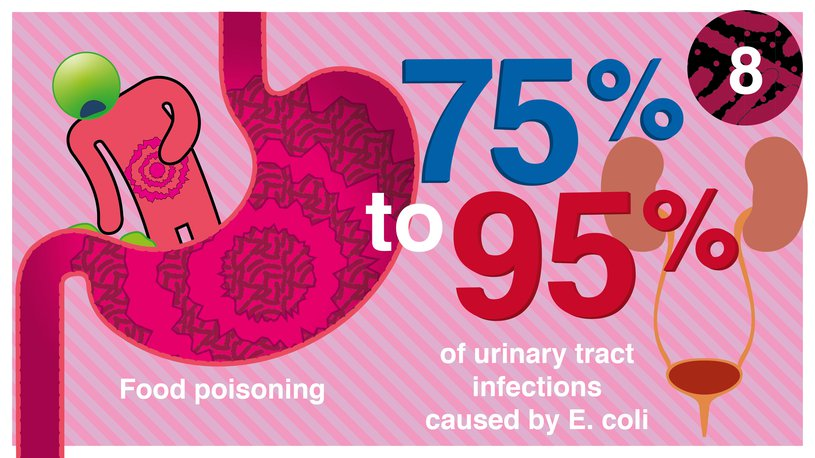
Although most forms of E. coli are harmless, the pathogenic strains can cause illness most commonly associated with food poisoning . Diarrhoea is a common symptom and for most people this subsides after a few days.
However, 75- 95% of urinary tract infections are caused by E. coli and in roughly 5-10% of cases it can lead to HUS, which can cause problems with the kidneys and even be life threatening. Young children and the elderly are among the most high-risk groups.
As such, we shouldn’t be complacent when it comes to E. coli. With proper hygiene and food safety standards , outbreaks can be avoided or severely reduced.
Discover the key information and food safety advice for managing E. coli. Download the Pal Hygiene infographic by clicking the link below.